Nursing Education Articles & Guides

3 Mins Read04 Jun 25
Thinking about becoming a nurse and want a program that reflects your values? Faith based Accelerated BSN (ABSN) programs are…

3 Mins Read04 Jun 25
If you already have a bachelor's degree and are ready for a meaningful career shift, New York's Accelerated BSN (ABSN)…

9 Mins Read16 May 25
In today’s diverse healthcare landscape, the ability to communicate in multiple languages has evolved from a beneficial skill to an…

11 Mins Read03 May 25
Advanced Practice Registered Nurses (APRNs) in Texas must complete specific continuing education (CE) requirements to maintain licensure and remain current…

11 Mins Read02 May 25
Registered nurses looking to advance their careers, increase their earning potential, and specialize in areas they’re passionate about often turn…
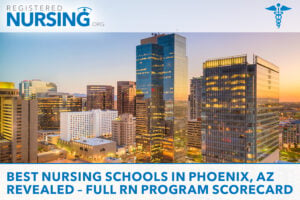
8 Mins Read29 Apr 25
Phoenix Nursing Programs – 2024 NCLEX First-Time Results Phoenix's nursing programs are preparing students for success, with a total of…

10 Mins Read26 Apr 25
Labor and delivery (L&D) nurses work on the front lines of one of healthcare's most dynamic and meaningful specialties—helping families…
9 Mins Read24 Apr 25
As the demand for qualified nurses continues to grow, so does the emphasis on patient safety, regulatory compliance, and workforce…

12 Mins Read22 Apr 25
Selecting the right capstone project is a pivotal moment in any nursing student’s academic journey. As the culminating experience of…

12 Mins Read16 Apr 25
Certified Nurse Midwives (CNMs) occupy a unique position in healthcare, blending clinical expertise with a deeply personalized approach to women’s…

3 Mins Read15 Apr 25
Returning from deployment, a military nurse reenters American soil with a wealth of experience but also a complex road ahead,…
Nursing Careers & Specialties Articles & Guides

9 Mins Read16 May 25
In today’s diverse healthcare landscape, the ability to communicate in multiple languages has evolved from a beneficial skill to an…

10 Mins Read05 May 25
The Advanced Practice Registered Nurse (APRN) Consensus Model is a regulatory framework designed to standardize how APRNs are educated, licensed,…

11 Mins Read02 May 25
Registered nurses looking to advance their careers, increase their earning potential, and specialize in areas they’re passionate about often turn…
11 Mins Read01 May 25
Private duty nursing is a growing and in-demand field offering a highly personalized approach to patient care. In 2025, as…

12 Mins Read25 Apr 25
California faces unique healthcare challenges that directly impact which nursing specialties are most critically needed throughout the state. From the…
9 Mins Read24 Apr 25
As the demand for qualified nurses continues to grow, so does the emphasis on patient safety, regulatory compliance, and workforce…

11 Mins Read21 Apr 25
In today’s dynamic healthcare landscape, nurses often need to secure licensure swiftly to meet urgent staffing demands. Whether you’re a…

11 Mins Read19 Apr 25
The United States is facing a critical and persistent shortage of registered nurses—a growing concern that significantly impacts patient care,…

11 Mins Read17 Apr 25
Registered nurses with extensive clinical experience and specialized knowledge possess valuable expertise that can significantly impact legal proceedings. As an…

12 Mins Read16 Apr 25
Certified Nurse Midwives (CNMs) occupy a unique position in healthcare, blending clinical expertise with a deeply personalized approach to women’s…

3 Mins Read15 Apr 25
Returning from deployment, a military nurse reenters American soil with a wealth of experience but also a complex road ahead,…
Nursing Life Articles & Guides

10 Mins Read05 May 25
The Advanced Practice Registered Nurse (APRN) Consensus Model is a regulatory framework designed to standardize how APRNs are educated, licensed,…

11 Mins Read30 Apr 25
Working from home isn't just for tech professionals—nurses now have expanding opportunities to bring their clinical expertise into home-based roles.…
9 Mins Read24 Apr 25
As the demand for qualified nurses continues to grow, so does the emphasis on patient safety, regulatory compliance, and workforce…

12 Mins Read31 Mar 25
The United States continues to face a nationwide nursing shortage, and internationally educated nurses are helping bridge the gap. For…

8 Mins Read25 Feb 25
Retirement from nursing doesn't mean the end of professional fulfillment. Many retired registered nurses (RNs) find that they still have…

12 Mins Read03 Jan 24
What Is a Travel Nurse? A travel nurse is a registered nurse (RN) who accepts temporary assignments—usually lasting a few…

5 Mins Read29 Sep 23
After many opportunities and encouragement from your leadership team, you have decided to plunge into nursing leadership. Whether your first…

5 Mins Read19 Sep 23
The 24/7, 365 care delivery model is a reality for many nurse leaders. That's why I like to say that…

5 Mins Read19 Sep 23
Nurses and nurse leaders want to work "gigs." Sometimes, it's money the desire to try something new, and other times,…

4 Mins Read01 Sep 23
Truth bomb: My ADN program in the 1980s did not teach me ANYTHING about budgeting for a department. Aseptic technique…

5 Mins Read29 Aug 23
What is a mentor? If you search the internet, the first definition it pulls up simply states "an experienced and…
Nursing Articles & Guides Archives
2022 Articles
- NP, DNP, and Ph.D. in Nursing: How High-Level Nursing Salaries Compare to MD Salaries [Updated 2025]